Nearly everything you need to know about mental health.
The Basics of Mental Health
Mental Health Is...
Mental health is our emotional, psychological, and social well-being. It is how we think, feel, and act. It helps determine how we handle stress, relate to others, and make healthy choices. Just like our physical health, it is important to all people at any age group.
Mental Illness Is...
Mental illnesses are conditions that affect a person’s thinking, feeling, mood or behavior in a way that impairs their ability to relate to others and function each day. Examples include MDD (depression) and schizophrenia. Poor mental health and mental illness are not the same thing. A person can experience poor mental health and not be diagnosed with a mental illness. Likewise, a person diagnosed with a mental illness can experience periods of good physical, mental, and social well-being.
Why is mental health important for overall health?
Mental and physical health are equally important components of overall health. Mental illness, especially depression, increases the risk for many types of physical health problems, particularly long-lasting conditions like stroke, type 2 diabetes, and heart disease. Similarly, the presence of chronic conditions can increase the risk factors and exacerbate the symptoms of mental illnesses like Depression or Bipolar Disorder.
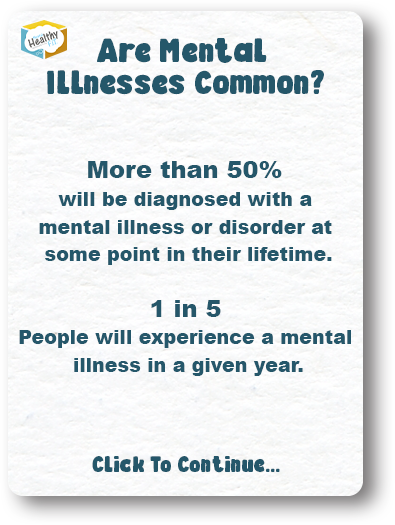
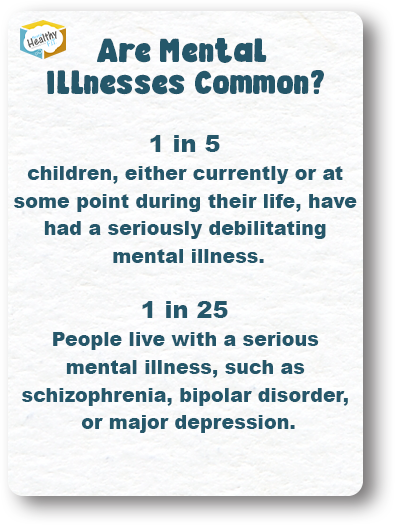
Are Mental Illnesses Common? (Spoiler Alert, Yes They Are)
More than 50% will be diagnosed with a mental illness or disorder at some point in their lifetime. 1 in 5 People will experience a mental illness in a given year. 1 in 5 children, either currently or at some point during their life, have had a seriously debilitating mental illness. 1 in 25 People live with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression.
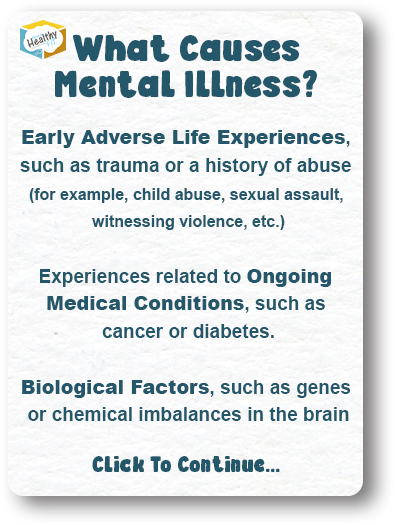
What Causes Mental Illness? Multiple Factors.
Early adverse life experiences, such as trauma or a history of abuse (for example, child abuse, sexual assault, witnessing violence, etc.) Experiences related to ongoing medical conditions, such as cancer or diabetes. Biological factors, such as genes or chemical imbalances in the brain Drug or alcohol abuse Social isolation, or reinforced feelings of lonliness
A Deep Dive Into Mental Health and Mental Illness
People experience different types of mental health issues, and they can occur at the same time. Mental illnesses can occur in short bursts, or extended episodes, then subside. Mental illnesses can also be ongoing, chronic conditions. There are more than 200 types of mental illness. Some of the main types of mental illness and disorders, but we will cover a handful of them in this deep dive.
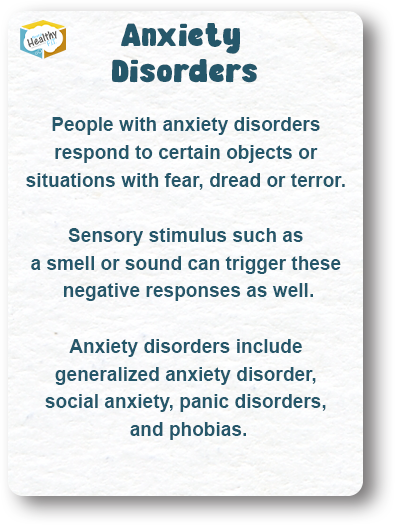
Anxiety Disorders
People with anxiety disorders respond to certain objects or situations with fear, dread or terror. Sensory stimulus such as a smell or sound can trigger these negative responses as well. Anxiety disorders include generalized anxiety disorder, social anxiety, panic disorders, and phobias.
Attention-Deficit/ Hyperactivity Disorder
ADHD is one of the most common childhood mental disorders. It can continue through adolescence and adulthood. People diagnosed with ADHD may have trouble paying attention, controlling impulsive behaviors, or be overly active to the point of self detriment.
Disruptive Behavioral Disorders
Behavioral disorders involve a pattern of disruptive behaviors in children that last for at least 6 months and cause problems in school, at home, and in social situations. Behavioral symptoms can also continue into adulthood, with the disruptive behavoirs becoming implusive to the point of serious self detriment.
Mood Disorders Such as Depression and Bipolar disorders
While bad moods are common, and usually pass in a short period, people suffering from mood disorders live with more constant and severe symptoms. Their mood impacts both mental and psychological well-being, nearly every day. 1 in 10 adults suffer from some type of mood disorder, with the most common conditions being depression and bipolar disorder. If left untreated, this illness can affect role functioning, quality of life and many long-lasting physical health problems such as diabetes and heart disease. With proper diagnosis and treatment, most of those living with mood disorders lead healthy, normal and productive lives. Many go undiagnosed, making mental health awareness a social imperative.
Eating Disorders
Eating disorders involve obsessive and sometimes distressing thoughts and behaviors concerning food and/or body image, including: • Reduction of food intake
Overeating
Feelings of depression or distress
Concerns or delusions about weight, body shape, poor self-image (Body Dysmorphia)
Common types of eating disorders include anorexia, bulimia, and binge eating.
Personality Disorders
People with personality disorders have extreme and inflexible personality traits that cause problems in work, school, or social relationships. Sharp and sudden personality changes can also be present. Personality disorders include antisocial personality disorder and borderline personality disorder (BPD).
Posttraumatic Stress Disorder (PTSD)
PTSD can manifest after living through a traumatic event, such as war, a natural disaster, abuse, or a serious accident. PTSD can make someone feel stressed and afraid after the danger is over. People with PTSD may experience symptoms like reliving the traumatic event, sleep problems, suffer from panic attacks, paranoia, and changes in emotions. PTSD can cause irritability, emotional outbursts, helplessness, or feelings of numbness.
Schizophrenia Spectrum and Other Psychotic Disorders
People with psychotic disorders hear, see, and believe things that aren’t real or true. They may also show signs of disorganized thinking, confused speech, and abnormal motor behavior. An example of a psychotic disorder is schizophrenia, which can also present disorganized motivation and emotions.
Substance Use Disorders
Substance use disorders occur when frequent or repeated use of alcohol and/or drugs causes significant detriment, such as health problems, disability, and failure to meet major responsibilities. Substance use problems can be fatal to the user and put others at risk. Examples include drunk driving and overdoses. Mental illnesses and substance use disorders often occur together. Sometimes one disorder can be a contributing factor to or can make the other worse. Sometimes they simply occur at the same time.
The Facts
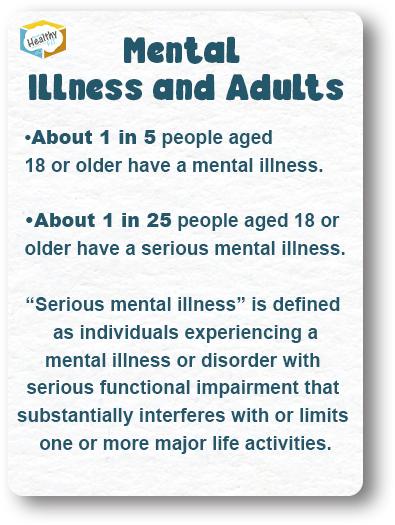
Mental Illness and Adults…
About 1 in 5 people aged 18 or older have a mental illness.
About 1 in 25 people aged 18 or older have a serious mental illness. “Serious mental illness” is defined as individuals experiencing a mental illness or disorder with serious functional impairment that substantially interferes with or limits one or more major life activities.
Mental Illness and Children and Teens…
1 in 5 – children, have had a seriously debilitating mental disorder.
Half of all chronic mental illness begins by age 14 and three-quarters begin by age 24.
The Social and Economic Impact of Mental Illness…
Suicide, often associated with symptoms of mental illness, is the 10th leading cause of death the U.S. and the 2nd leading cause of death among people aged 15-34.
Serious mental illness costs the United States $193.2 billion in lost earnings per year.
Mood disorders, including major depression, dysthymic disorder, and bipolar disorder, are the third most common cause of hospitalization in the United States. for both youth and adults aged 18 to 44.
Individuals living with serious mental illness face an increased risk of physical health problems, such as heart disease, diabetes, and HIV (human immunodeficiency virus, the virus that causes AIDS).
U.S. adults living with serious mental illness die on average 25 years earlier than others, largely due to treatable medical conditions.
Mental Health Promotion and Prevention…
Preventing mental illness and promoting good mental health involves actions to create living conditions and environments that support mental health and allow people to adopt and maintain healthy lifestyles. These include a range of actions to increase the chances of more people experiencing better mental health, such as...
Early childhood interventions (for example, home visits for pregnant women and programs that help young children build social and emotional skills).
Social support for the elderly.
Programs targeted to people affected by disasters, war, abuse or other traumatic events. •Mental health interventions at work (for example, stress prevention programs).
Violence prevention strategies (for example, reducing violence in the community and the home). •Campaigns to change the culture of mental health so that those in need receive the care and support they deserve.
Educate yourself on all aspects of mental health
Stigma
9/10 people with a mental health issue experience stigma and discrimination
Stigma can be understood in terms of three components: stereotypes, prejudice, and discrimination.
Stigmas surround mental illness. The only way to avoid them is to first understand them. They include having fixed ideas and judgments about mental illness and/or fearing and avoiding what is misunderstood. Stigma can appear as attitudes (thoughts and prejudices) and/or behaviors (bullying, avoidance, violence, etc.). There are significant consequences of feeling stigmatized. They can include limiting a person’s ability to attain and keep a job or safe place to live, reducing a person’s desire to seek treatment and support, fears of not being accepted by family, friends or the larger community, and avoiding relationships or social activities. The prejudice and discrimination felt by those with mental health issues might lead to believing these negative stereotypes, resulting in feelings of shame and guilt. We must be compassionate and thoughtful when talking about mental illness, using accurate and sensitive words.
Anxiety
Anxiety disorders are the most common mental illnesses, affecting 18% of the population
Anxiety is the most common mental illness out there, and it takes a lot of different forms. Experiencing some level of anxiety is a normal part of being human, but for people who have an anxiety disorder the worry or fear do not go away, and worsen over time. Some people experience generalized anxiety, where the negative thoughts and feelings are present in a variety of circumstances, while others experience social anxiety, anxiety in crowds, and sexual anxiety, just to name a few. Anxiety can cause intense and prolonged feelings of fear and distress that occur out of proportion to the threat or danger at hand. Thankfully, anxiety is treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms. That being said, many people have found successful treatment for anxiety through things like psychotherapy (often Cognitive-Behavioral Therapy), support groups, medication, spiritual and indigenous approaches to healing, and stress management and relaxation techniques.
ADHD
Approximately two-thirds of children with ADHD will not meet the criteria for ADHD diagnosis as adults
Attention Deficit Hyperactive Disorder (ADHD) frequently begins in childhood. People who live with ADHD can have trouble paying attention, might not be able to determine the “appropriate” amount of physical activity for a given situation, act before thinking, and find themselves daydreaming. They also find it hard to focus, organize, and finish tasks. ADHD is treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms for dealing with ADHD. That being said, many people have found successful treatment for ADHD through various types of psychotherapy, medication, behavioral interventions, education and training, mindfulness, and spiritual and indigenous practices. Usually folks with ADHD have better outcomes when they combine more than one type of treatment.
Bipolar Disorder
At least half of all cases of bipolar disorder start before age 25
Bipolar Disorder causes unusual changes in mood and behavior. While everyone has natural highs and lows, with bipolar disorder the highs and lows are extreme, impacting individuals’ ability to function in their day-to-day lives. Intense shifts in mood, energy levels, sleeping and eating, and the ability to think clearly are all signs of Bipolar Disorder. Mania or hypomania (extreme highs) in addition to depression are key components of being diagnosed with the disorder. In between episodes, people with Bipolar Disorder can be completely symptom-free. Like all mental illnesses, Bipolar Disorder shows up differently for each person. For example, some people could be in either a manic and/or depressive state almost all the time, whereas for others it could be years between episodes. Bipolar Disorder is treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms for dealing with bipolar disorder. That being said, many people have found successful treatment for bipolar through things like psychotherapy, medication, exercise, spiritual and indigenous approaches to healing, and/or self-care techniques such as sticking to concrete daily routines or keeping a journal to track symptoms.
Borderline Personality Disorder
Almost half of people who are diagnosed with BPD will
not meet the criteria for diagnosis just two years later.
Ten years later, 88% of people who were diagnosed
with BPD no longer meet the criteria for a diagnosis
Borderline Personality Disorder (BPD) causes dramatic changes in someone’s moods, behaviors and relationships. Often, people with BPD have a strong desire to be close with someone, but also have an inability to trust that person, so their relationships can be a constant push and pull of “please stay here with me” and “get away from me.” Because people with BPD have a hard time regulating their emotions, they can take impulsive actions driven by extreme shifts in mood. Anger morphs into depression, which evolves into elation, all within just a few hours. Borderline personality disorder is treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms for dealing with BPD. That being said, many people have found successful treatment for borderline through a combination of things including psychotherapy (especially Dialectical Behavioral Therapy or DBT), medication, trauma-sensitive work, spiritual and indigenous practices, and family and partner support. Sometimes extreme stress, leading to a lack of impulse control, can require a person with BPD to take care of themselves by checking into the hospital for safety and support.
Depression
Young adults aged 18–25 are 60% more likely to have
depression than people aged 50 or older
Depression causes severe, negative changes in the way you think and feel, making it difficult to manage day-to-day tasks and activities such as working, sleeping, and/or eating. Many people with depression feel numb, sad, alone, and/or like life has no meaning. Some people will only have one depressive episode in their lifetime, but for many people depression recurs and episodes can last up to several years if untreated. Episodes of depression may occur with or following stressful events, physical illnesses, trauma, loss, major transitions and financial stress. They can also happen for no discernible “reason.” It can be constant, or it can come and go with time, events, or seasons. Depression is treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms for dealing with depression. Many people have found successful treatment for depression through things like support groups, medication, psychotherapy, exercise, spiritual and indigenous approaches to healing, and herbal supplements.
Eating Disorders
incidence of anorexia in young women 15-19 have risen in each decade since 1930
Eating disorders are a group of conditions that cause serious emotional and physical problems, involving extreme food and weight issues. There are many types of eating disorders (anorexia, bulimia, binge eating disorder, etc.), and while they vary greatly in what they look like, they all point to an unhealthy, and sometimes dangerous relationship to food. Eating disorders are treatable.
Each person is unique, and should explore their options and select for themselves the most effective coping mechanisms for dealing with an eating disorder. That being said, many people have found successful treatment for ED through things like psychotherapy, support groups, medication to treat depression or anxiety if co-occurring, nutritional counseling, family-based treatment, and/or spiritual and indigenous approaches to healing.
Obsessive Compulsive Disorder (OCD)
Approximately 2.3% of the population between ages 18-54 suffers from OCD
Obsessive-Compulsive Disorder (OCD) is a specific form of anxiety characterized by repetitive, unwanted intrusive thoughts (obsessions) and irrational, excessive urges to do certain actions (compulsions). For some people, the compulsive behavior comes from trying to reduce anxiety or obsessions. Genetics tend to play an important role; if you, your parent or a sibling have OCD, there is almost a 25% chance that another family member will have it.
OCD can look different for different people; for some, it involves cleaning self and spaces compulsively; for others, the OCD might present in the form of counting, tapping, or something numeric, or a myriad of other forms.
Each person is unique, and should explore the options and select for themselves the most effective coping mechanisms for dealing with OCD. That being said, many people have found successful treatment for OCD through things like psychotherapy (specifically a form of Cognitive-Behavioral Therapy called Exposure and Response Prevention delivered one-on-one or in group settings), medication, exercise, and/or spiritual and indigenous approaches to healing.
PTSD
94% of survivors of sexual violence experience PTSD symptoms during the first 2 weeks following the assault
Post Traumatic Stress Disorder (PTSD) is a response to a traumatic event or series of events. Something that is traumatic for one person might not be traumatic for another, but what matters is how that experience stays with the person. It can include flashbacks to the traumatic event, uncontrollable movements and thoughts, anxiety and hyper vigilance, physical and emotional triggers, among other symptoms.
PTSD is most commonly found among survivors of sexual violence, as well as war veterans, survivors of abuse or natural disasters, and witnesses to violence. Not all traumatic experiences lead to PTSD and there are many factors that affect the severity, such as the number of other traumatic experiences in a person’s life, their reaction to the event, and the kind of support they received after.
It is extremely important to take your feelings seriously and learn to treat and manage symptoms. There are a lot of approaches to working with PTSD, including psychotherapy (an approach specifically designed to work with trauma is EMDR – Eye Movement Desensitization and Reprocessing), medication, sharing in community, support groups, somatic interventions around triggers, and spiritual and indigenous approaches to healing.
Addiction
About a third of all people experiencing mental
illnesses and about half of people living with severe
mental illnesses also experience substance abuse.
About a third of all alcohol abusers and more than half
of all drug abusers report experiencing a mental
illness
Substance abuse refers to the harmful use of psychoactive substances, including alcohol and drugs. Substance use can lead to addiction and dependence, creating a condition in which the body requires a drug in order to function without physical and psychological reactions to its absence. Persistent and repeated substance use typically leads to a strong desire to take the drug, difficulty in controlling its use, and persisting in its use despite harmful consequences.
People can experience addiction to substances, as well has behaviors such as gambling, sex, or engaging in extreme situations. Addiction can quickly take over a person’s life and can become more important than the need to eat or sleep, replacing things that the person used to enjoy. There is a strong correlation between substance abuse/addiction and mental illness, often referred to as a Dual Diagnosis. More than half of the people with addiction issues also experience mental health issues, as they affect the same parts of the brain.
Treatment approaches vary, and choosing the appropriate type depends on the severity and addiction itself. Treatment can include support groups, harm reduction and safer use, psychotherapy, medication, spiritual and indigenous practices, and holistic approaches.
Suicide
White males accounted for 7 out of every 10 suicides in
2014. The rate of suicide is highest in middle age
white men in particular
Suicidality can be experienced by anyone. Approximately 90% of individuals who die by suicide experience a mental illness, making it an issue closely tied to what we do here at Mental Healthy. There are infinite reasons why someone might feel like killing themselves is the only option. Factors that may put a person at risk of suicide include: substance abuse, chronic medical illness, oppression due to an identity (such as race, gender, sexual orientation, religion, etc.), history of trauma, isolation, sleep deprivation and age (under 24 or above 65 are at a higher risk).
To reduce the danger of suicide, psychotherapy and medication can be used to help recognize unhealthy patterns of thinking and teach coping skills to deal with problems. Seeking treatment for underlying depression and anxiety through doctors or health professionals is essential, as is building social and peer support networks. The most important thing to remember is that you are not alone, and help is available. Call the National Suicide Prevention Lifeline at 1-800-273-8255.
If you are concerned about someone, talk with them and ask them directly if they are thinking about suicide and if they have a plan to end their life. If this is the case, connect with a crisis service and stay with the person, listening without judgement and telling them they are important and you care about them.